guide
Introducing Predictive Document Intelligence
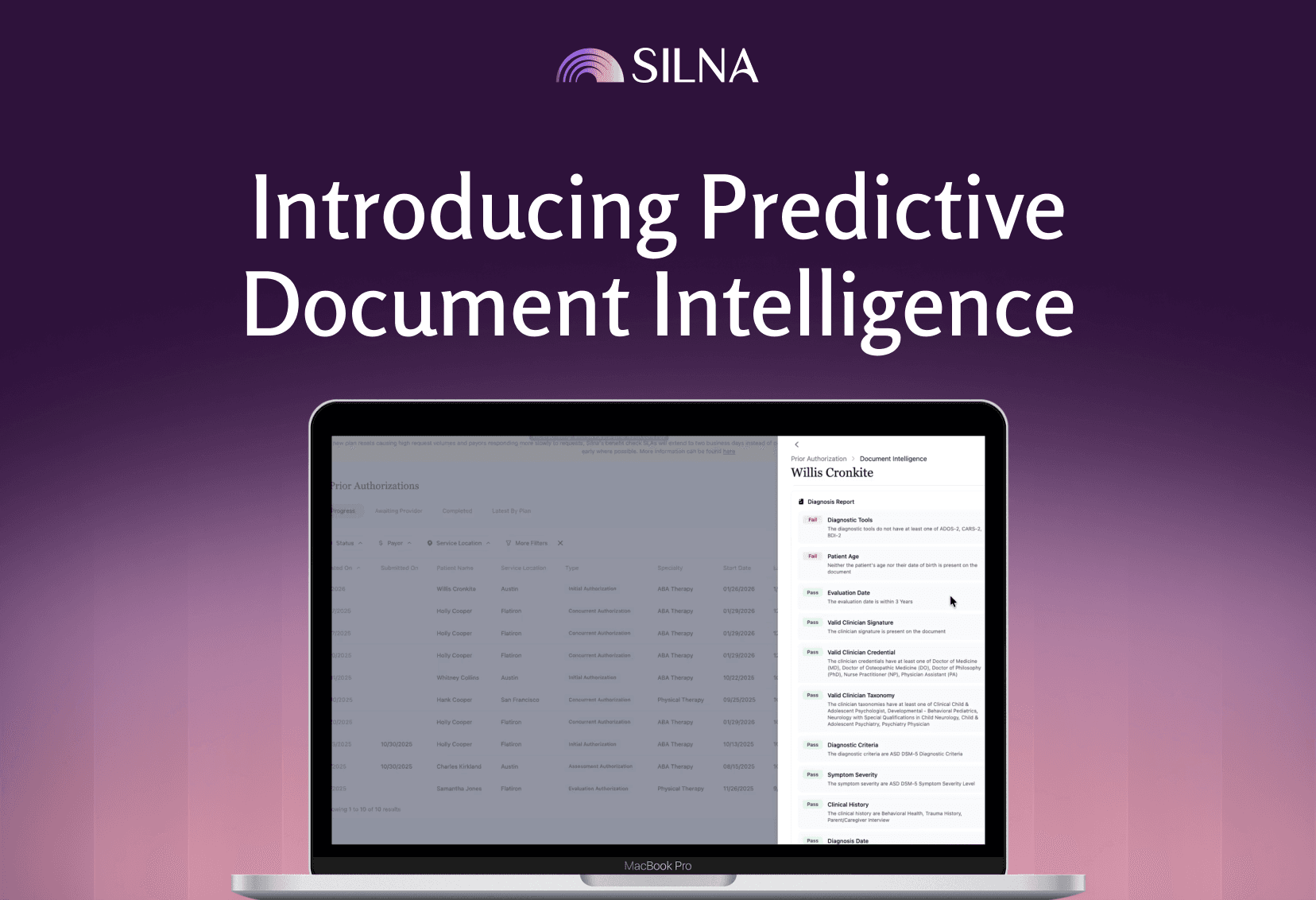
Since launching Silna last April, Silna has grown to support over 150,000 patients nationwide and become the #1 rated prior authorization solution on G2. Today, we’re taking the next step with Predictive Document Intelligence, our first AI-powered capability designed to prevent prior authorization denials before they happen.
We’re excited to share about this launch, which is now part of Silna’s Care Readiness Platform.
Why prior authorization keeps failing patients
Despite years of policy debate and incremental reform, prior authorization continues to delay or deny care for millions of patients across the U.S. According to the American Medical Association, prior authorization delays care for 94% of patients, and in more than 82% of cases, it contributes to patients abandoning treatment entirely.
Most of the time, the delay doesn’t come from a clinical disagreement. It comes from paperwork that isn’t quite right. A form is missing a signature. A document is outdated. A requirement changed and no one caught it. By the time the issue surfaces, the request has already been denied and the patient is left waiting.
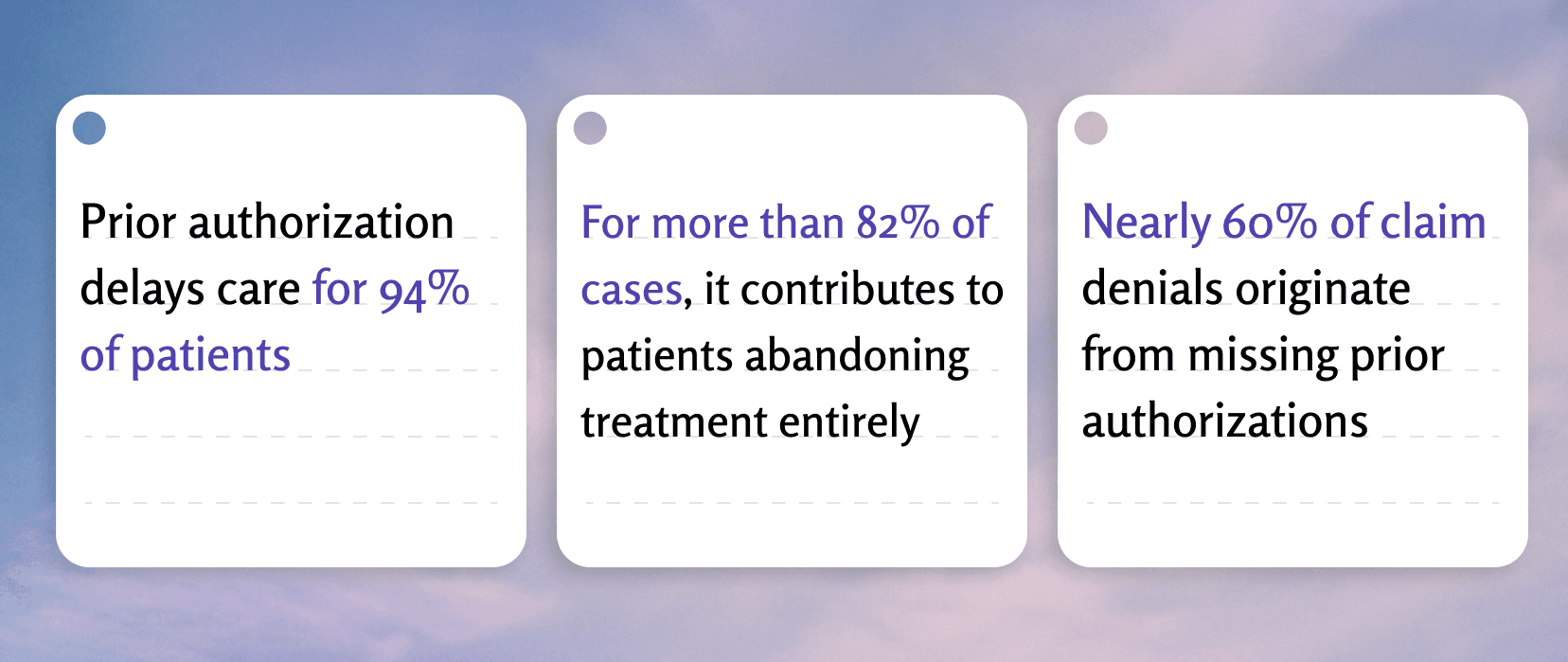
What’s often overlooked is why so many authorizations fail. Nearly 60% of claim denials originate from missing prior authorizations, minor documentation inaccuracies–such as specific language requirements or missing signatures–outdated eligibility, or other front-end administrative failures, not from the claim itself.
These failures happen before a patient ever receives treatment. And once they happen, fixing prior authorizations is slow, manual, and often requires significantly more work for the provider compared to the initial authorization submission.
The hidden failure point: documentation readiness
Most authorization workflows today are built around submission, not readiness.
Providers gather clinical documentation, fill out payor forms, and submit requests without truly knowing whether the documentation meets payor- and specialty-specific requirements. When a denial comes back days or weeks later, teams are forced into costly rework.
The reality is that payors operate with highly specific, constantly changing rules:
- Required documentation varies by payor, plan, state, specialty, and procedure
- Minor inconsistencies: missing dates, outdated assessments, mismatched diagnoses, specific outcome measures not listed can all trigger denials
- Requirements are rarely transparent or surfaced clearly within provider workflows
Until now, providers have had no practical way to evaluate documentation quality at scale before submission.
What we built
Predictive Document Intelligence was built to address this exact gap.
Instead of asking, “Why was this authorization denied?” Silna asks a more important question upfront: “Is this patient actually clear to receive care?”
Predictive Document Intelligence evaluates clinical documentation before submission to determine whether it is complete, consistent, and aligned with what a specific payor requires for approval. When issues are identified, then they’re flagged, and that’s when they’re easiest to fix.
This includes:
- Validating documentation against a continuously updated library of payor-specific rules
- Identifying missing, outdated, or inconsistent clinical information
- Surfacing issues that commonly lead to denials before requests are submitted
- Providing clear guidance to resolve gaps proactively
Here’s what this looks like in practice: Before Predictive Document Intelligence, a provider might submit a prior authorization request and wait 5-7 days only to receive a denial because a psychiatric evaluation was dated outside the payor’s 90-day window. Now, that issue is caught before submission, allowing the provider team to request an updated evaluation without delaying care. Prior authorizations requests submitted using this technology are accepted 24.5% faster, and prior authorizations validated with the platform achieve a 98% first-pass acceptance rate.
From reactive workflows to proactive care readiness
Predictive Document Intelligence is part of Silna’s broader Care Readiness Platform, which takes a fundamentally proactive approach to front-end insurance workflows.
Instead of managing authorizations after problems arise, Silna helps providers handle all required checks upfront:
- Are benefits active and accurate?
- Is prior authorization required?
- Does the documentation meet payor requirements?
- Is the patient truly cleared to receive care?
When these questions are answered early, authorization workflows stop being a bottleneck and start becoming a source of confidence.
Over time, consistently high-quality submissions don’t just reduce denials. They also help providers demonstrate reliability to payors, which is increasingly important in programs like gold carding, where applicable.
Alongside this new capability, Silna’s platform includes our Prior Authorization API, which integrates directly into provider workflows to surface submission criteria in real time, and a team of experienced authorization specialists to handle edge cases and payor-specific nuances that automation alone can’t solve.
Why this matters for patients
Administrative delays are often a patient access problem.
When documentation is incomplete or authorizations are denied, patients wait. Treatments are postponed. In some cases, care is abandoned entirely.
By preventing denials before they occur, Predictive Document Intelligence helps ensure that patients receive the care they need when they need it without unnecessary friction or uncertainty.
This is what care readiness looks like in practice: fewer surprises, fewer delays, and a system that works the first time.
“Silna’s document intelligence feature provides an extra layer of review to ensure diagnostic report accuracy, helping us prevent authorization denials,” said Nichole Joyce, Senior Director at AnswersNow. “It allows us to quickly catch and correct issues before care begins, minimizing delays for our clients.”
Looking ahead
Predictive Document Intelligence builds on Silna’s recent momentum as we continue to invest in eliminating fragmented, manual insurance workflows. With more than 150,000 patients supported nationwide, our focus remains the same: replacing reactive, error-prone processes with intelligent infrastructure that improves access to care.
If you’re a healthcare provider dealing with constant prior authorization denials, or if you’re interested in joining our mission to fix healthcare’s administrative burden, we’d love to hear from you.
—
Jeffrey Morelli
Co-Founder & CEO, Silna